In the world of orthobiologics, there’s a fascinating and complex interaction between different types of cells that significantly impact the effectiveness of therapies like Platelet-rich plasma (PRP), a common treatment that promotes healing in tissues like cartilage and bone.
However, not all PRP is created equal, and the presence of specific white blood cells, called neutrophils, can greatly affect its effectiveness.
Neutrophils: The Double-Edged Sword
Neutrophils are white blood cells that play a crucial role in our immune system. Neutrophils are among the first responders to the injury site when our body is harmed. They release enzymes and reactive molecules to fight infection and clean up damaged tissue. However, in the context of PRP therapy, this aggressive response can sometimes do more harm than good.
How Neutrophils Affect PRP Therapy
- Breaking Down Essential Tissues: Neutrophils release enzymes that can degrade vital components of tissues. For instance, they can break down collagen and other essential molecules in cartilage and bone. This degradation can weaken cartilage in conditions like osteoarthritis and impair bone healing after fractures.
- Causing Oxidative Stress: Neutrophils produce reactive oxygen species (ROS), which can lead to oxidative stress. This stress damages cells’ lipids, proteins, and DNA, worsening inflammation and hindering the body’s natural repair processes.
- Sustaining Chronic Inflammation: Neutrophils release inflammatory molecules that keep inflammation going. In conditions like osteoarthritis, this persistent inflammation can prevent proper tissue healing and even lead to the formation of fibrous tissue instead of healthy, functional tissue.
- Degrading Growth Factors: PRP is rich in growth factors crucial for our healing. However, neutrophil enzymes and ROS can degrade these growth factors, reducing their effectiveness and compromising the healing process.
The Drawbacks of Leukocyte-Rich PRP
Leukocyte-rich PRP (LR-PRP) contains high levels of white blood cells, including neutrophils. While it might seem beneficial to have these immune cells present, studies have shown that LR-PRP can increase cell death and promote the release of more inflammatory molecules, exacerbating inflammation rather than helping with healing.
The Advantage of Leukocyte-Poor PRP
To address these issues, researchers have developed techniques to create leukocyte-poor PRP, which minimizes the presence of neutrophils. This type of PRP is prepared using methods that reduce tissue trauma during blood collection, optimize centrifugation to separate platelets from white blood cells, and focus on preserving the beneficial growth factors while avoiding the adverse effects of neutrophils.
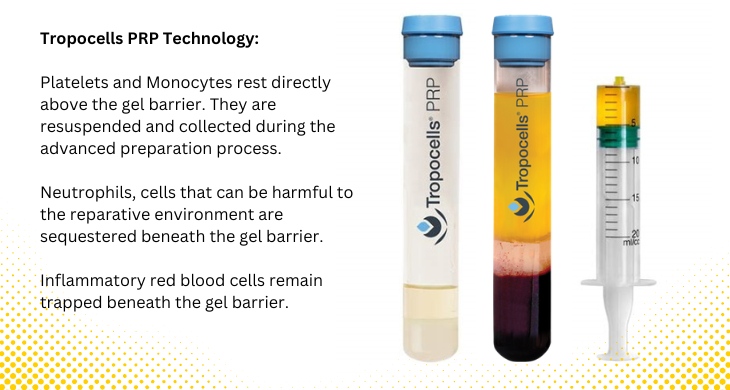
Tropocells Gel Separator PRP Tubes: Enhancing PRP Quality
An innovative approach to minimizing neutrophil contamination is the use of gel separator PRP tubes. These tubes contain a special gel that forms a barrier during centrifugation, effectively separating different blood components. Here’s how they work:
- Minimizing Neutrophil Contamination: The gel barrier helps to keep neutrophils and other unwanted cells away from the platelet-rich plasma layer. This separation ensures that the final PRP product contains fewer neutrophils, reducing the risk of inflammation and tissue damage for the patient.
- Removing Red Blood Cells: Gel separator tubes can remove up to 99% of red blood cells from the PRP. Red blood cells are not needed in PRP therapy, and their removal further purifies the PRP, enhancing its therapeutic potential for the patient.
Tropocells Technology: A Step Ahead
One advanced technology in this field is Tropocells PRP. This system has been engineered to remove more than 95% of neutrophils while retaining a high concentration of platelets. The result is a PRP formulation rich in platelets and beneficial monocytes but low in inflammatory neutrophils. This approach enhances the healing potential of PRP by reducing inflammation and preserving the bioactivity of growth factors.
Why Buffy Coat Systems Fall Short
Older PRP preparation systems, known as buffy coat systems, often fail to separate neutrophils from platelets adequately. While these systems can provide PRP with high platelet concentrations, they also include significant levels of neutrophils, which can hinder the healing process. In contrast, advanced systems like Tropocells are specifically designed to optimize the composition of PRP for better therapeutic outcomes.
Conclusion
While the most important factor in predicting positive outcomes is platelet dose, the presence of neutrophils in PRP can significantly impact its effectiveness. By minimizing neutrophil contamination and optimizing platelet dose, advanced PRP preparation techniques, such as those used in Tropocells PRP technology, can enhance the therapeutic potential of PRP therapy in orthopedic and regenerative medicine. This careful balance between harnessing the benefits of platelets and avoiding the drawbacks of excessive inflammation is critical to achieving better healing and improved patient outcomes.